Fixing the Failed Restoration: Provisional and Placement
My patient wasn’t satisfied with the esthetics and feel of her previous restoration. Detailed planning enabled me to deliver a beautiful, functional result. Here is the conclusion of this case and placement of the new six unit anterior bridge:
Failed Restoration: Provisional
After the treatment planning was completed, I removed the patient’s existing anterior bridge and replaced it with a bisacryl provisional derived from the orthodontic wax-up. I sectioned it specifically to enable tooth movement while I restored the pontic sites. This meant sectioning between the maxillary central, the upper left lateral and central, and the upper right canine and lateral.
I then cemented the provisional with Rely-X luting cement. Doing so decreased displacement secondary to the orthodontic forces. Next, the patient went through orthodontic therapy over three months. Following this, she was ready for periodontal surgery. Crown lengthening was done on the upper right canine, in addition to placing connective tissue grafts in the pontic sites. This ensured ovate pontics could develop.
Failed Restoration: Equilibration & Placement
Equilibration was the natural next step. It was used to achieve the necessary anterior guidance with posterior disclusion, as well as freedom in the anterior and no centric occlusion slide to maximum intercuspal position.
I prepped off the orthodontic provisional and refined the preparation. For the margin design, I went with a shoulder and rounded internal line. This could accommodate the all-porcelain restorations.
We weren’t worried about the reduction of 1.5 mm because of the original tooth reduction, but we did go forward with placement of a third plane of reduction. This was necessary for final incisal edge placement in a AP dimension.
Venus from Hereaus was used to create the six unit provisional from upper right to upper left canine. This also allowed tissue development to occur in the pontic sites.
After taking final impressions three months later, the six unit bridge was made using E.max. I placed the patient’s direct composite veneers on the upper first molars and bicuspids. Shade matching to the anterior bridge was one advantage of this approach. Also, the patient could choose to move to porcelain at some point in the future.
My patient was finally happy with her smile. All in all, it took dedicated teamwork between myself, the ceramist, orthodontist, and periodontist to exceed her expectations.
Related Course
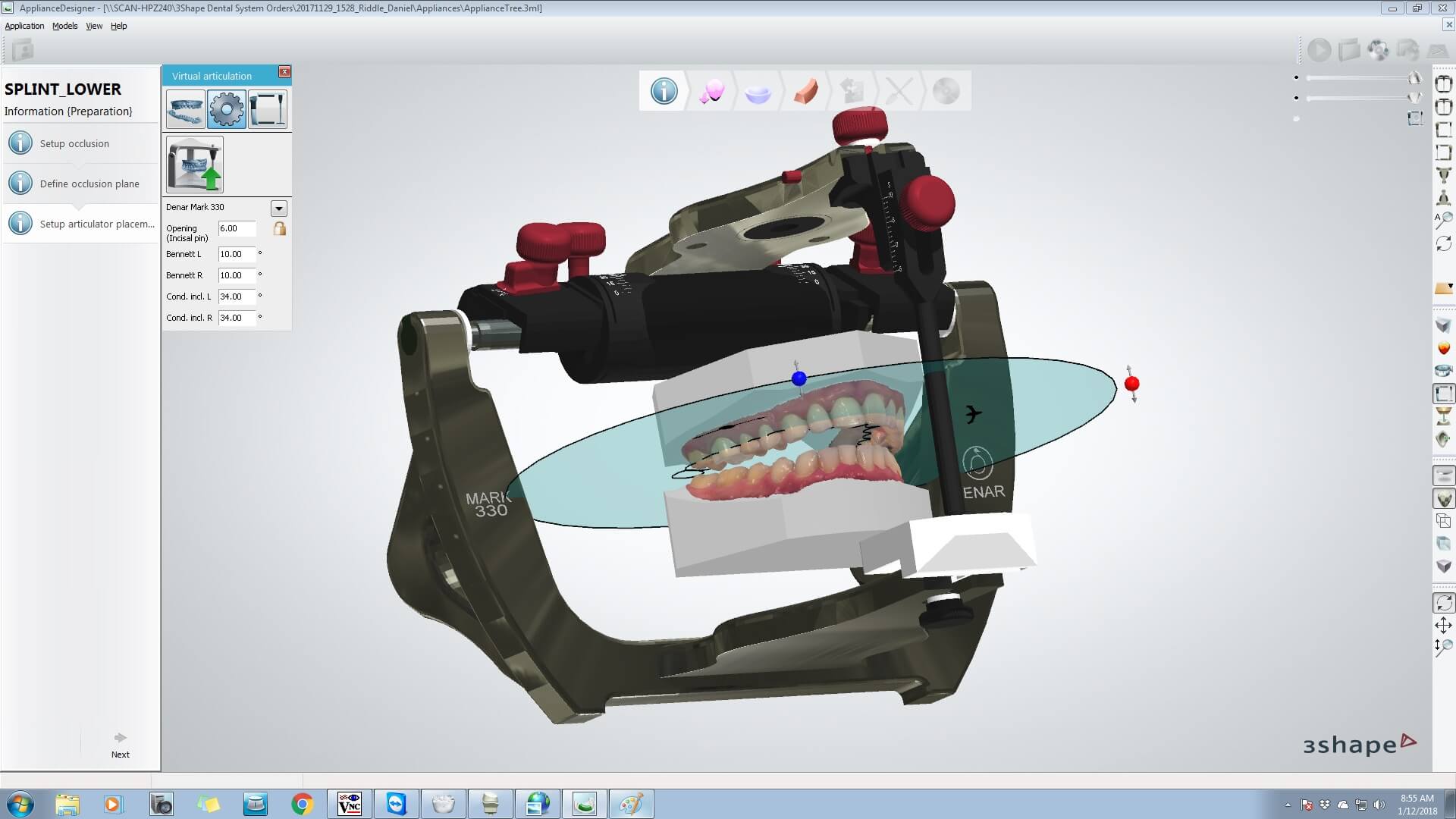
Mastering Advanced Splint Therapy
DATE: November 13 2025 @ 8:00 am - November 16 2025 @ 1:00 pmLocation: The Pankey Institute
CE HOURS: 29
Dentist Tuition : $ 5900
Single Occupancy with Ensuite Private Bath (per night): $ 345
If you are ready to take what you know about appliance therapy to the next level, then this course is a must. The anatomic appliance is one of the most…
Learn More>