Dental Sleep Medicine in Restorative Practice Part 5: Selecting Appliances
Dental Sleep Medicine in Restorative Practice Part 5: Selecting Appliances
By Todd Sander DMD
This article is written for dentists who are thinking about or just starting a dental sleep medicine practice. I do both restorative dentistry and dental sleep medicine, and by sharing what I do, I hope to help others with their planning.
There are many other types of appliances you can consider and I am always looking at them. But to become most efficient, I have narrowed down the types of appliances I deliver. Most commonly, these are Dorsal and Herbst appliances. Both are titratable, as the patient needs more advancement over time..
The dorsal appliance resembles a custom-fitted mouthguard, worn only during sleep. It uses advancement blocks with an orthodontic screw to advance the jaw. There are many manufacturers, and it is easy to deliver. It doesn’t impinge on the tongue, so patients find it comfortable. It is fairly durable and repairable, especially if milled out of acrylic. This is my go-to type of appliance for most patients because patients respond favorably to them.
A Herbst appliance is more durable for parafunctional patients and fairly comfortable. Patients are sometimes intimidated when they first look at this type of appliance but I always point out that the advancement bars are in the dead space of the cheeks, and they won’t feel them. There are many types of Herbst appliances with different types of advancement arms.
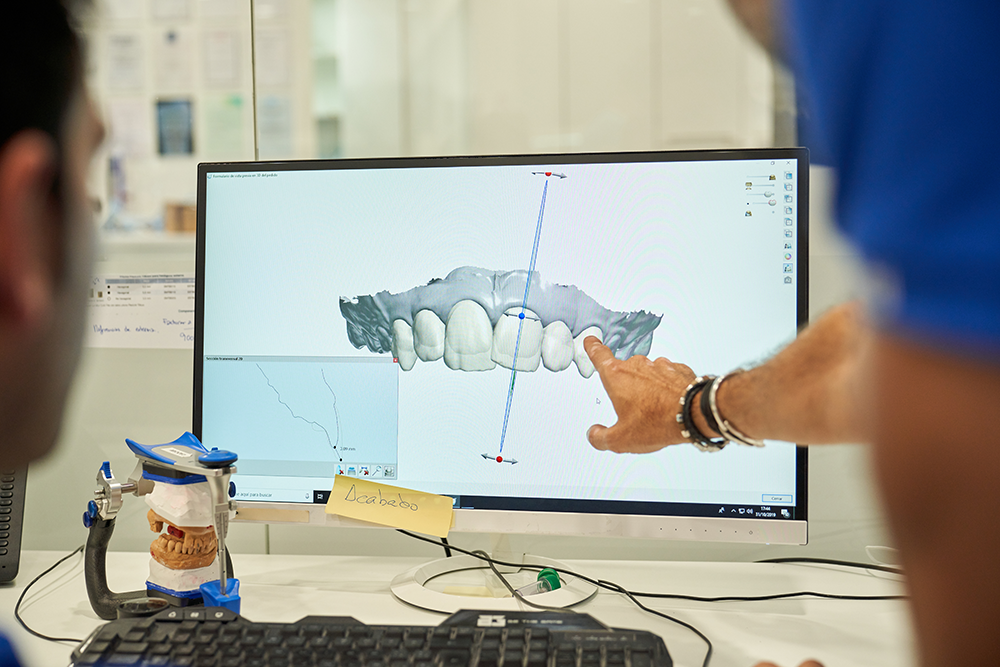
I sometimes deliver an EMA appliance or a TAP 3 appliance. I have found that the screw and bar assembly of TAP appliances can impinge the tongue a little. My preference is to use appliances that provide more room for the tongue to move forward. Milling and 3D printing have introduced many low-profile, stable, and comfortable appliances that deserve investigation.
Whatever appliance you decide to use, become knowledgeable and proficient with it. You want to convey confidence to your patients. The more they trust in the appliance, the more compliant they will be with wearing it and the sooner they can achieve improvement of their sleep breathing issues. Oftentimes, they will feel better within a week or two and report this during their first recall visit. When they report improved symptoms, we can move on to confirming the treatment position with a home sleep monitor and refer them back to their physician. Treatment position can also be confirmed prior to appliance fabrication by using a MyTAP temporary appliance. This can improve the initial treatment position and is necessary for non-titratable appliances..
With most patients, we take two steps forward and one step back as we titrate an appliance to an effective treatment position. Sometimes I need to send an appliance back, so I’ve become used to taking a bite registration myself and sending it to the lab to reset the appliance in a more forward position. Using a MyTAP to determine treatment position ahead of time helps prevent this. We prepare our patients for this possibility and provide encouragement to stay on course. Working as a team with our patients, we will get there!
Related Course
TMD & Orofacial Pain: Managing Complex Patients
DATE: January 29 2025 @ 8:00 am - February 2 2025 @ 1:00 pmLocation: The Pankey Institute
CE HOURS: 37
Dentist Tuition: $ 7200
Single Occupancy with Ensuite Private Bath (per night): $ 345
THIS COURSE IS SOLD OUT TMD patients present with a wide range of concerns and symptoms from tension headaches and muscle challenges to significant joint inflammation and breakdown. Accurate thorough…
Learn More>